Fast Facts: Tick Bites
By Jonathan Badger PharmD, MS
Published: Jul 10, 2024

Ticks are opportunistic parasites that wait perched at the tips of grass, weeds, or leaves for their next meal to brush up against them. If you are that unlucky person it means you are on the menu. In this fast facts article we will go over how to properly remove an attached tick, bite care and monitoring, and when to get your health care provider involved.
Sections
Afterbite care and when to get your doctor involved
How to remove a tick
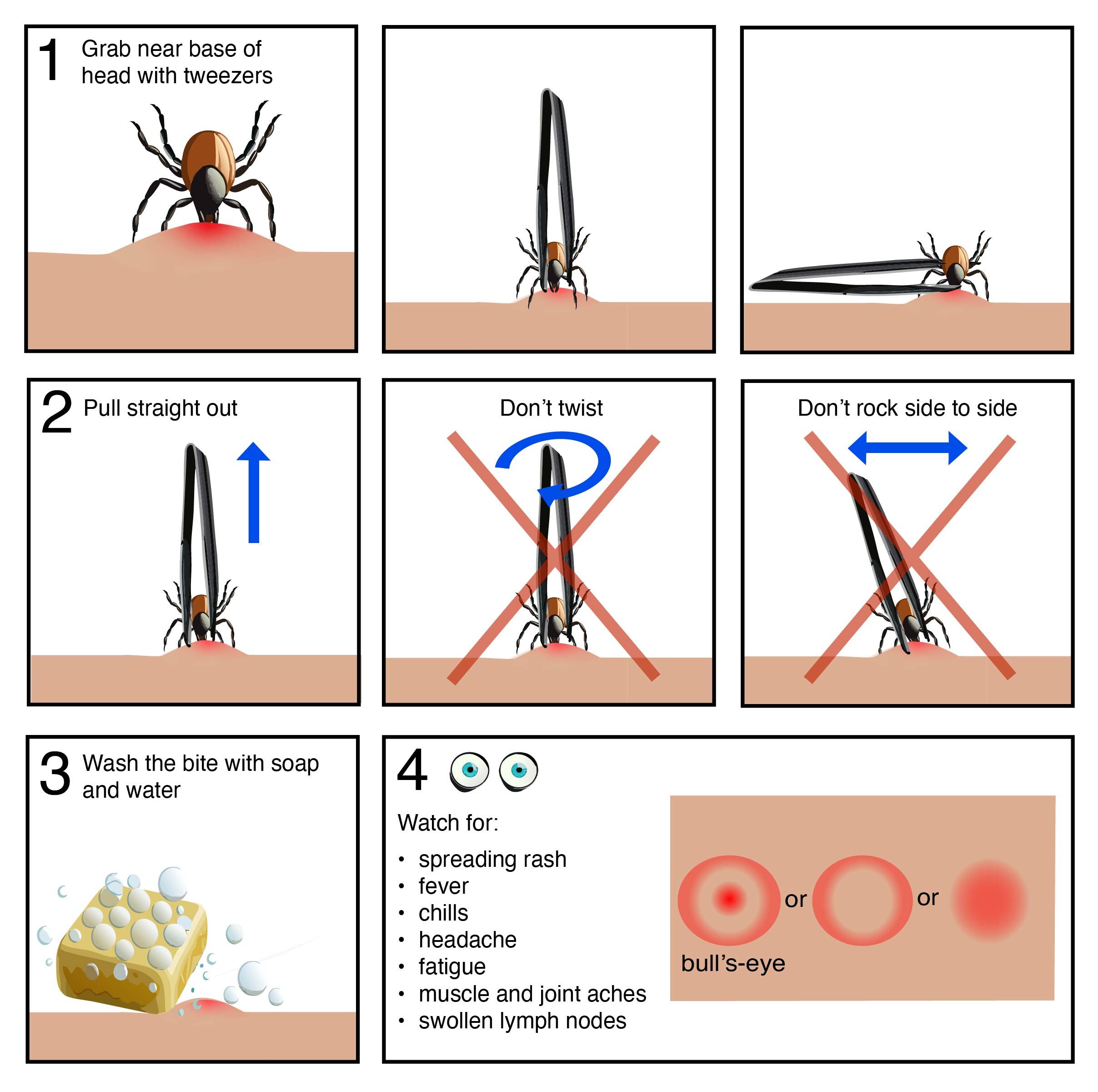
If you find a tick attached to your skin it’s important to remove it as soon as possible to prevent transmission of viruses or bacteria the tick may be carrying.
Using tweezers grab the tick near the base of the head as close to the skin as possible.
Using firm and even pressure pull straight out. Don’t twist or rock back and forth. Twisting and rocking can cause the head or mouthparts to break off and remain embedded in the skin. If after removing the tick there are mouth parts embedded in the skin, remove them with tweezers if you can, but don’t try and dig them out.
Wash the bite and your hands thoroughly with soap and water. You can also use isopropyl alcohol to disinfect the bite if you have it handy.
Monitor the bite. If you develop a rash or start to feel sick within a few weeks of getting bitten by a tick get seen by a healthcare professional. (more details below)
Removal Methods to avoid
- trying to burn the tick using a lighter, cigarette, or hot end of a blown out match
- trying to smother the tick so it 'backs out' using olive oil, vaseline, nail polish, or something similar
- squeezing and/or crushing the tick
Book keeping
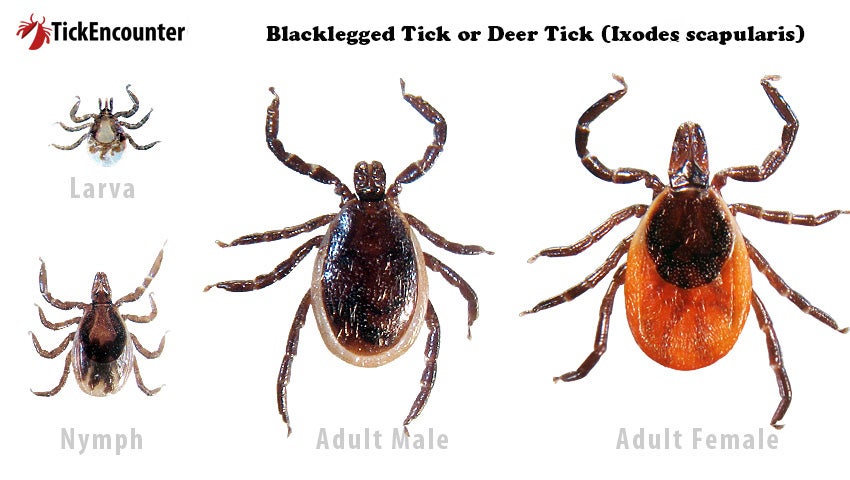
Consider putting a few notes in your phone about your tick encounter. Take a picture of the tick, especially if you are unsure what kind it is. The species of tick and its appearance (flat versus fat and engorged with blood) can be used to help steer medical decisions by your doctor should you need to be seen. Record the date you removed the tick and the date you think you were first bitten or were out in tick habitat.
Disposal
After washing the bite with soap and water you should dispose of the tick. The toilet or a sealed ziploc bag placed in the garbage are good options.
Afterbite care and when to get your doctor involved
It’s common for tick bites and the immediate surrounding area to be a little red and itchy for a few days. If the head or mouthparts from the tick are left behind itching and irritation are more likely to be intense. A thin film of hydrocortisone 1% cream 3-4 times per day can help.
Monitoring
Most tick bites resolve on their own, but ticks can transmit bacteria and viruses that can make you sick, so monitoring after a tick bite is important.2 If you develop a rash, fever, or other symptoms of severe illness in the first few weeks to a month after getting bitten get seen by your doctor.
The development of a rash can be an early warning sign of infection for Lyme disease and Rocky Mountain Spotted fever, but doesn’t appear in all cases. If you don’t have a rash but have other symptoms you should still get seen.
The other symptoms to watch out for are flu-like and include fever, chills, headache, fatigue, muscle and joint aches, and swollen lymph nodes.
Lyme Disease
Lyme disease, the most common illness you can catch from ticks, is caused by a bacteria that’s carried in deer ticks (also called blacklegged ticks). Deer ticks mainly live in the eastern half of the US and most cases of Lyme disease occur in the upper midwest and north eastern states.
Rash and early signs
In the early stage of Lyme disease (3 to 30 days after being bitten) a rash around the area of the bite is very common (70-80% of cases).2 It often looks like a target or a bull’s eye, but the appearance can vary.
Other early symptoms include fever, chills, fatigue, malaise, headache, achy muscles, achy joints, and swollen lymph nodes.
Seek prompt treatment if any of these occur after a tick bite.
Antibiotic prophylaxis
If you live in an area where Lyme disease is common antibiotics are sometimes prescribed to prevent illness. Use the map below to help determine if you are in a high risk area.
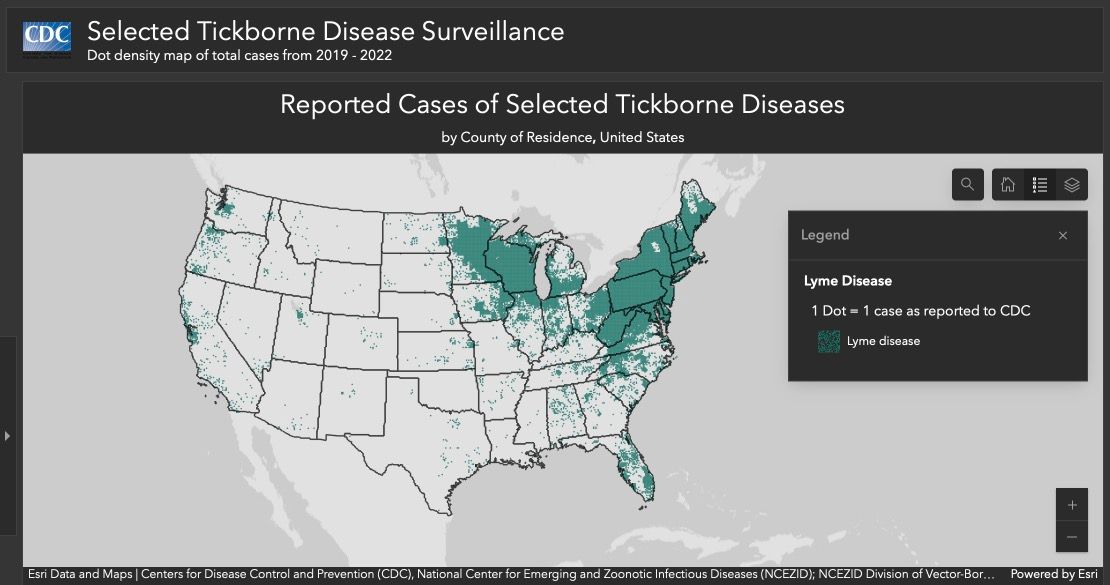
The guidelines for use of prophylactic antibiotics are fairly stringent, but if you were bitten by a deer tick in a high risk area, the tick was engorged with blood, and you just removed it consider talking with your doctors office or local urgent care to see if pretreating with antibiotics is an appropriate option for you.
References
Krinsky DL, Ferreri SP, Hemstreet B, et al. Handbook of Nonprescription Drugs: An Interactive Approach to Self-Care. 20th ed. American Pharmacists Association; 2021.
Center for Disease Control. Tickborne Diseases of the United States[Internet]. Atlanta (GA) US Center for Disease Control; Sixth Edition 2022 [cited 2024 July 10]. Available from: https://www.cdc.gov/ticks/tickbornediseases/TickborneDiseases-P.pdf.